When carbohydrates are consumed, digested, and absorbed the pancreas senses the subsequent rise in blood glucose concentration and releases insulin to promote an uptake of glucose from the blood stream. When insulin binds on the cellular insulin receptor, it leads to a cascade of cellular processes that promote the usage or, in some cases, the storage of glucose in the cell. The effects of insulin vary depending on the tissue involved, e.g., insulin is most important in the uptake of glucose by muscle and adipose tissue.
This insulin signal transduction pathway is composed of trigger mechanisms (e.g., autophosphorylation mechanisms) that serve as signals throughout the cell. There is also a counter mechanism in the body to stop the secretion of insulin beyond a certain limit. Namely, those counter-regulatory mechanisms are glucagon and epinephrine. The process of the regulation of blood glucose (also known as glucose homeostasis) also exhibits oscillatory behavior.
On a pathological basis, this topic is crucial to understanding certain disorders in the body such as diabetes (type 1,2,3), hyperglycemia and hypoglycemia.
Insulin signal transduction pathway
The functioning of a signal transduction pathway is based on extra-cellular signaling that in turn creates a response which causes other subsequent responses, hence creating a chain reaction, or cascade. During the course of signaling, the cell uses each response for accomplishing some kind of a purpose along the way. Insulin secretion mechanism is a common example of signal transduction pathway mechanism.
Insulin is produced by the pancreas in a region called Islets of Langerhans. In the islets of Langerhans, there are beta-cells, which are responsible for production of insulin. Insulin is secreted as a response mechanism for counteracting the increasing excess amounts of glucose in the blood.
Glucose in the body increases after food consumption. This is primarily due to carbohydrate intake, but to much lesser degree protein intake ([1])([2]). Depending on the tissue type, the glucose enters the cell through facilitated or passive diffusion. In muscle and adipose tissue, glucose enters through GLUT 4 receptors via facilitated diffusion ([3]). In brain, kidney and retina, glucose enters passively. In the beta-cells of the pancreas, glucose enters through the GLUT 2 receptors (process described below).
Two aspects of this process are explained below: insulin secretion and insulin action on the cell.
Insulin secretion
The glucose that goes in the bloodstream after food consumption also enters the beta cells in the Islets of Langerhans in the pancreas. The glucose passively diffuses in the beta cell through a GLUT-2 vesicle. Inside the beta cell, the following process occurs:
Glucose gets converted to Glucose-6-Phosphate (G6P) through Glucokinase; and G6P is subsequently oxidized to form ATP. This process inhibits the ATP sensitive potassium ion channels of the cell causing the Potassium ion channel to close and not function anymore. The closure of the ATP-sensitive potassium channels causes depolarization of the cell membrane causing the cell membrane to stretch which causes the voltage-gated calcium channel on the membrane to open causing an influx of Ca2+ ions. This influx then stimulates fusion of the insulin vesicles (bubble like structure with insulin in them) to the cell membrane and secretion of insulin in the extracellular fluid outside the beta cell; thus making it enter the bloodstream.
Insulin action on the cell
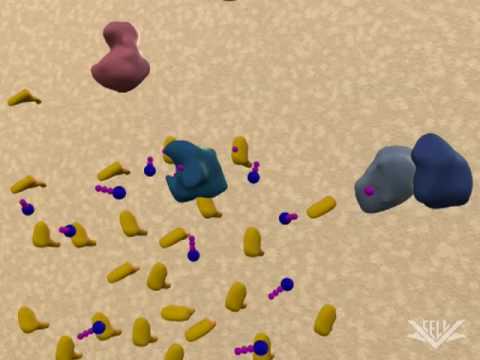
After insulin enters the bloodstream, it is taken up by the cells, as glucose is the preferential fuel for human bodies. However, insulin does not directly go inside the cell in its original form. To activate the effects of insulin, it has to bind to an enzyme that activates its functions. Thus, the insulin binds to the α (alpha) subunit of the insulin receptor embedded in the cell membrane. The α-subunit acts as the insulin receptor and the insulin molecule acts as a ligand in an receptor-ligand complex.
This triggers the tyrosine kinase activity in the β-subunit that is attached to the α-subunit. The tyrosine kinase activity causes phosphorylation (activation) of the enzymes.
The 2 enzymes, Mitogen-activated Protein Kinase (MAP-Kinase) and Phosphatidylinositol-3-Kinase (PI-3K, Phosphoinositide 3-kinase) are responsible for expressing the mitogenic and metabolic actions of Insulin respectively.
The activation of MAP-Kinase leads to completion of mitogenic functions like cell growth and gene expression.
The activation of PI-3K leads to crucial metabolic functions such as synthesis of lipids, proteins and glycogen. It also leads to cell survival and cell proliferation. Most importantly, the PI-3K pathway is responsible for the distribution of glucose for important cell functions. The GLUT-4 vesicle (responsible for passive diffusion of glucose in cell) binds to the PI-3K after bringing glucose in the cell. The PI-3K isolates the GLUT-4 Vesicle from the glucose and sends the vesicle back to the cell membrane. The glucose that is isolated is then sent to the mitochondria to make ATP and excess glucose is stored in the cell as glycogen. [This process is also illustrated in Figure 1.1.2].[2]
Thus, insulin’s role is more of a promoter for the usage of glucose in the cells rather than neutralizing or counteracting it.
Wikipedia contributors. "Insulin signal transduction pathway and regulation of blood glucose." Wikipedia, The Free Encyclopedia. Wikipedia, The Free Encyclopedia, 15 Sep. 2015. Web. 25 Oct. 2015.